Vertigo Deep Dive: BPPV
BPPV is one of the most common types of vertigo.
BPPV is actually an acronym that stands for:
Benign, meaning BPPV is not life-threatening;
Paroxysmal, meaning, transient. The symptoms come and go rapidly;
Positional, because this vertigo is triggered by changes in head position;
Vertigo, as patients experience dizziness/spinning symptoms.
What is it? BPPV is a type of vertigo caused by a dysfunction of the vestibular system, located on either side of your head next to the hearing apparatus. People with BPPV commonly report strong dizziness symptoms when lying back in a dentist’s chair, getting their hair cleaned at the salon, or when rolling over in bed; in a study, patients who indicated "YES" on the Dizziness Handicap Inventory for rolling over in bed and getting out of bed were highly likely to have a BPPV diagnosis[1].
Vestibular Anatomy
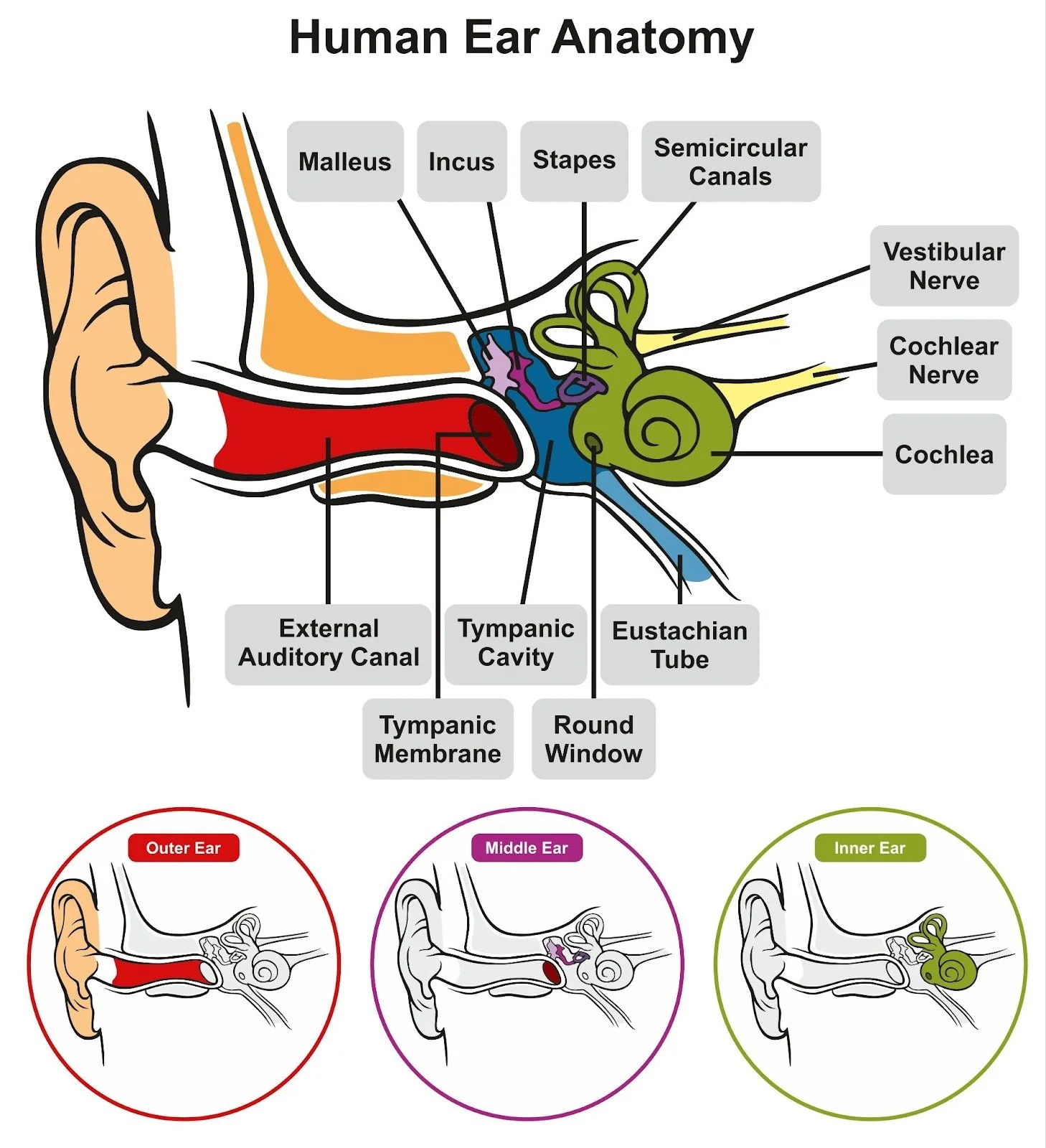
The study of BPPV helps us further understand vestibular anatomy and why we see the symptoms we do. It is important to understand the main purpose of the vestibular system: detect motion of the head, and communicate that information to the brain. To accomplish this, the highly specialized vestibular system deep within your inner ear consists of two otolith organs (utricle, saccule) and three semicircular canals, pictured in Figure 1, on each side of your head. For BPPV, let’s hone in on those semicircular canals and their function. The semi-circular canals are filled with a thick, viscous fluid, and at the entrance of each canal is the ampulla, which is home to a special detector called the cupula. Think of the cupula like a bell that rings whenever the fluid in the canal pushes against it, telling the brain the 411.
So, how do the canals detect movement?
Think about what happens when you turn a jar of honey upside-down to sweeten your tea: the bottle moves first, and the slower fluid eventually catches up. When you turn your head to the left, the canals (and the cupula) move with your head, faster than the thick fluid moves. The movement of the cupula through the thick fluid deflects it in the opposite direction of movement, ringing that bell. Think about what happens to your hair as you swim laps in the pool--the force of the water pushes your hair in the opposite direction of your movement. The deflection of the cupula sends a nerve impulse to the brain to tell it what happened! But, just like the honey, the fluid does move. Once that fluid starts moving leftward, it deflects the cupula in the opposite direction.
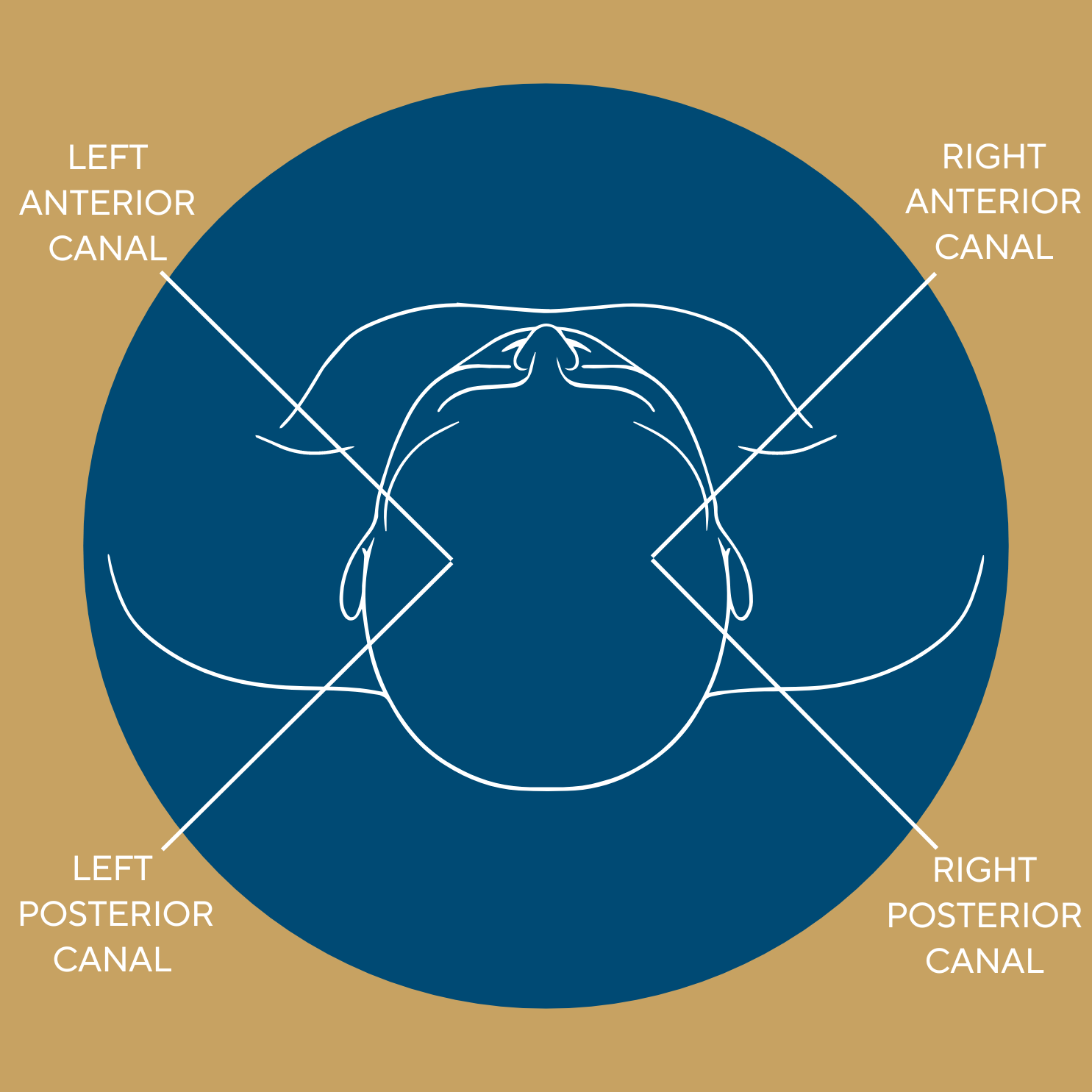
Each of the three canals (horizontal, anterior, and posterior) are oriented 90 degrees from each other, allowing them to detect motion in all possible planes. The posterior and anterior canals are vertically aligned and positioned 45 degrees from midline (see diagram). The posterior and anterior canal of opposite sides, as well as both left and right horizontal canals, are co-planar, meaning they are oriented in the same plane. This is a useful redundancy in case the system on one side is working less optimally than the other, as is the case with vestibular hypofunction.
The Vestibular System & Vision
So, why does our body have this system in place? One of the overarching purposes of these canals is to detect position changes of the head, and relay that information to the brain so that it can stabilize your vision. When the head moves, the brain tells the eyes to move in the opposite direction to allow you to keep your eyes on target. Try it: focus your eyes on something and move your head around—for most, the object remains clear even though you’re moving your head. This specific phenomenon is called the vestibulo-ocular reflex (VOR) that pairs head and eye movements. This point is important, because one of the symptoms of BPPV involves eye movement.
Back to BPPV
Unfortunately, sometimes debris—called otoconia—can break off from other parts of the vestibular system and wander into the fluid filled semicircular canals where they don’t belong. Canalithiasis, which is much more common, means the otoconia remains suspended in the canal fluid. Cupulolithiasis means the debris gets stuck on the cupula.
In the case of canalithiasis, when the head changes position, gravity exerts a force on the debris, causing it to fall towards the bottom of the canal in its new position, even as the canal (and fluid within) has stopped. Symptoms begin when the fluid has stopped moving on its own, but the debris hasn't, so it can take a few seconds for someone to feel symptoms after the change in position has occurred. This migration of debris exerts a pressure on the fluid, pushing on it, causing inappropriate deflection of the cupula, making the detector turn back on even though we’ve stopped moving! This mismatch in signals from the vestibular system and other parts of the body, including vision, makes you feel very dizzy. The debris is slogging through this viscous, honey-like material to get to the bottom of the canal—so our symptoms can last anywhere from a few seconds to up to a minute. When the debris settles and stops pushing on the fluid, the symptoms ease.
For cupulolithiasis, the debris weighs down the detector, causing it to deflect even if there is no longer relative movement between the canals and the fluid. Clinical pearl: Cupulolithiasis symptoms tend to happen immediately (zero latency) with head position changes because it directly affects the deflection of the cupula, whereas patients with canalithiasis start to experience symptoms a few seconds after the change in position
Nystagmus & BPPV
In addition to making you feel super dizzy, when debris moves through the canal, the brain falsely believes the head is moving—therefore, it attempts to stabilize vision through that aforementioned VOR. As a result, the brain works on this misinformation to move the eyes in the opposite direction of the "head movement". The brain is smart—it quickly realizes the information from the vestibular system is false, and it tries to correct this with a rapid correction of the eye position called a saccade. The cycle of aberrant eye movement triggered by the debris and the brain's correction is called nystagmus. Problem is, while the debris/junk keeps falling and deflecting that cupula, the brain continues this cycle of eye movement and correction until the debris has settled. In fact, the direction of the corrective saccade helps clinicians identify the affected canal so we can expedite treatment. For example, rightward "upbeating" nystagmus tells us the BPPV is in the right posterior canal.
Dix-Hallpike & Supine Roll Tests
Clinicians assess BPPV via the (1) right and (2) left Dix-Hallpike and (3) Supine Roll Tests. Remember the three canals, and their 90-90-90 orientation? These three tests position each of the three canals along the plane of movement to see which symptoms are produced. That helps narrow down which canal contains the debris! The Dix-Hallpike starts with an individual in long sitting, turning their head either right of left, then laying on their back in the "provoking" position with their head extended back off the edge of a table. In Figure 6 below, Jess is performing the Dix-Hallpike on herself to assess the right posterior canal, or, because they are co-planar, left anterior canal. Here, Jess turns her head 45 degrees to the right to position these canals in the plane of movement before lying back. The symptoms someone experiences in each position, combined with nystagmus latency, duration, and direction, can lead clinicians towards deducing the affected canal!
References
Whitney SL, Marchetti GF, Morris LO. Usefulness of the dizziness handicap inventory in the screening for benign paroxysmal positional vertigo. Otol Neurotol. 2005;26(5):1027-1033. doi:10.1097/01.mao.0000185066.04834.4e